Pearls of Wisdom and a Few Grains of Sand (v1)
This past week I was fortunate to attend the First Amsterdam Breech Conference in one of Europe’s most beautiful cities. There were two full days of speakers sharing their research, insights, experience and opinions. Unlike some papers and publications related to this topic which have blurred the lines between honest data and bias, the speakers here did their best to not muddy the line between research and opinion. Each was clear when presenting data and stressed the importance of methodology and comparing apples to apples versus offering information that would be considered Level C or opinion and presenting it as fact. What follows are from my notes with Dr. Stu commentary when appropriate.
We were welcomed by our hosts, Joris van der Post, MD PhD, Fedde Scheele, MD PhD and Ruth Evers, Midwife. “Safety” was discussed and, as you will see later in this blog, they acknowledged there is no clear definition of what this word means in our field. But there can be no substitute for experience and thus the purpose of this conference. Throughout the days we were treated to clips of some women sharing their birth stories and from Karin Ecker’s, “A Breech in the System” documentary. As if to put an exclamation point on the dichotomy that exists surrounding breech birth, Ruth Evers closed the conference by putting together a loop of 2 quotes from the obstetrician assisting Karin with her breech birth. “It’s never less than scary” she says while waiting for the labor to progress. And after the successful vaginal breech birth, “Why would anyone do it any other way”.
The inaugural talk was presented by Frank Louwen, MD PhD at Universitats-klinikum, Frankfurt, Germany. Dr. Louwen has long been recognized as a leader in breech delivery innovation and research and has trained many practitioners at his clinic. He titled his talk, “The re-invention of vaginal breech birth” (VBB). He stressed proper client selection and recognizing normal from pathological. With proper decision making he has found that blanket cesarean section policy can often increase the danger to mother and baby. “To do a surgery you need an indication!” he says. The majority of breech babies are a variation of normalcy, not pathology, and to perform surgery for normal is just wrong. Cesareans come with a whole list of problems which are often deemphasized in counseling. Increased maternal mortality, childhood asthma, diabetes and altered epigenetics to name a few. The Cochrane Data Base conclusions are changing from definitive in 2001 after the Term Breech Trial (TBT) was released to 2015 where “more information on safety of VBB is needed”. Dr. Louwen stressed that experts look at data and sometimes forget there is much more to consider.
An important point I had not considered before with regards to the TBT is the Dr. Hannah compared how vaginal delivery was done versus cesarean section. She noted the mode of delivery but not the technique. At the time, the mode of vaginal delivery for breech babies was nearly always in lithotomy which we now know can be a pathological position. So what were actually compared were the very standardized cesarean section technique and the pathological and unknown technique of VBB in the 1990s. Later in the conference many of the other methodology flaws of the TBT were introduced and I have written about them in earlier blogs. Dr. Louwen is an advocate of the “upright” or all fours position for VBB. In this position the umbilical cord is decompressed and gravity is of assistance. He also says that smaller babies increase the complication rate, not the big ones, as does pulling on the baby. His suggestion, “vaginal birth is superior to cesarean under physiologic circumstances and experienced companionship”. More from Frank later.
Betty-Anne Davis, RM MA, an adjunct professor and registered midwife at Carleton University in Ottawa, Canada next presented on the “Cardinal Movements and Crowning Touch”. Like many of these wonderful speakers, I’ve known Betty-Anne from previous breech conferences and it is always good when you are offering a service that seems out of the mainstream to be surrounded by friends and colleagues and receive affirmation that you are not alone. Using a model Betty-Anne reviewed the movements of a breech as it descends in and through the pelvis. Like cephalic babies there are basic cardinal movements that help the baby travel. An important point about feet presenting was made. When feet present but the hips and knees are flexed this is a complete breech and a vaginal birth is a reasonable decision. If, however, even one hip is extended then this is a footling breech and a cesarean is the better option. Just because a foot protrudes first does not define a footling! She also liked to say the small hands of a midwife might be an advantage for a maneuver she calls the crowning touch: Sliding in a single hand to assist flexion of the after coming head. She cannot recall the last time she saw use of Piper forceps at her institution. I will still carry them to my breech births although it has been several years since I used them. A reminder that we all develop our own comfort zones. And while often the adrenaline flows rich at a breech birth, for me it is rarely scary.
The next topic was on External Cephalic Version (ECV) presented by Marjolein Kok, MD PhD and Joost Velzel, MD PhD from the Netherlands and Mary Sheridan, RM MSc from London. All agreed an experienced operator was important. Women that underwent an ECV had a decreased rate of cesarean section which makes sense. Relative risk (RR) of 0.63%. They quote a 40-60% success rate. Data was presented that showed the only pharmaceutical agent with any benefit was terbutaline. There was no benefit found to oxytocin receptor blocker (Atosiban), Calcium channel blockers like Nifedipine or nitrates. Use of hypnosis was not mentioned but Dr. Louwen was kind enough to give me a reference where this has been looked at and found to be beneficial. This is important because most midwives are not able to use terbutaline in their practices. http://www.hindawi.com/journals/ecam/2012/626740/
Also, no mention of the value of an epidural which seems to be more and more in vogue but remains controversial: http://onlinelibrary.wiley.com/doi/10.1111/j.1471-0528.2000.tb13238.x/pdf
ECV was found to be most successful with: a relaxed uterus, unengaged breech, palpable head, multiparous client, posterior placenta, <65 kg. mother (143.3 lbs.), AFI > 10cm and complete breech position. Pretty much affirming what common sense would tell you. The only consensus contraindication to attempting an ECV is oligohydramnios. This from a review of 60 studies that discuss 39 contraindications but none of them evidenced based. Even a history of abruption, severe preeclampsia or a sign of fetal distress are only Level III (C) evidence of a contraindication to ECV. Complications included: abnormal CTE (FHR) tracing in 6.1%, fetal-maternal transfusion in 0.9% (Rhogam is usually given in Rh- mothers as the risk appears to be 1 in 100), emergency cesarean 0.35% (Each much assess the value of these numbers but I note that hospitals in my area usually perform ECV in an operating room for a 1/300 risk), stillbirth risk is 0.09%, placental abruption 0.08% and cord prolapse 0.3%. I just caution too much focus on the minutia of data. The experienced practitioner needs to alleviate anxiety and fear in the client which adds to the success of ECV, IMHO.
Gail Tully, Midwife and founder of Spinning Babies and a fellow Minnesotan (yay!) spoke next on visualizing obstructed breech birth. Hard to put in words what she demonstrates with models but suffice it to say her website has assisted thousands and has many pearls of wisdom. One good suggestion is to consider myofascial release before ECV.
The next lecture titled, “Risks, Rules & Reality” by Irene de Graaf, MD PhD and Rebekka Visser, Midwife provided an alternative way of looking at birth that needs to be continually reinforced. What is natural childbirth? They define it as instinctive human behavior in birth. The body, left to its own devices to work by itself. “Herbal is not natural. Home is not natural. Vaginal is not the definition of natural either.” Neither is hands and knees position. They state there is no research into what undisturbed birth is like. Which to me, reiterates one of the themes I felt running through this conference, that data on breech delivery constantly compares a standard cesarean to a nebulous, ill-defined option called vaginal breech delivery. At this point a premise known as Hitchens’s Razor was described. “What can be asserted without evidence can be dismissed without evidence” or what is freely asserted is freely deserted. Something I say all the time is that the concept of safety is often misused as a bludgeon by expert over layperson who then feels inadequate and bullied into unequal and sometimes unethical decision making. Lastly, they state that a woman who wants a physiologic birth deserves the same opportunity and consideration as one who wants a technological birth. The consensus seems to be to teach upright breech to midwives as they are in the best position in the Netherlands, at least, to handle the inevitable surprise breech when transport is not possible.
The last lectures of Day 1were a trilogy. Shared Decision Making and term breech in the Netherlands was presented by Floortje Vlemmix, MD PhD. For me, this lecture sparked some controversy and confusion in the audience when a slide was presented saying, “No longer is it justifiable for OBs to claim in their hands there is no increased fetal risk from vaginal birth”. Once again there was weight given to the TBT despite all the evidence of M. Glezerman and so many others. This was quite distressing but here is part of the argument as I understood it. The risk of perinatal death (number of stillbirths and deaths in the first week of life per 1,000 total births) with VBD is 1.6 and for planned cesarean it is 0.5. However, in a subsequent pregnancy the perinatal death risk is 1.3 /1000(multip) for VBD and 2.5/1000 for planned repeat cesarean. Thus, with a cesarean section in the first pregnancy the risk of a perinatal death after 2 pregnancies is equal to the risk from a VBD. So, for me and others, we are not sure of the point being made by the speaker here.
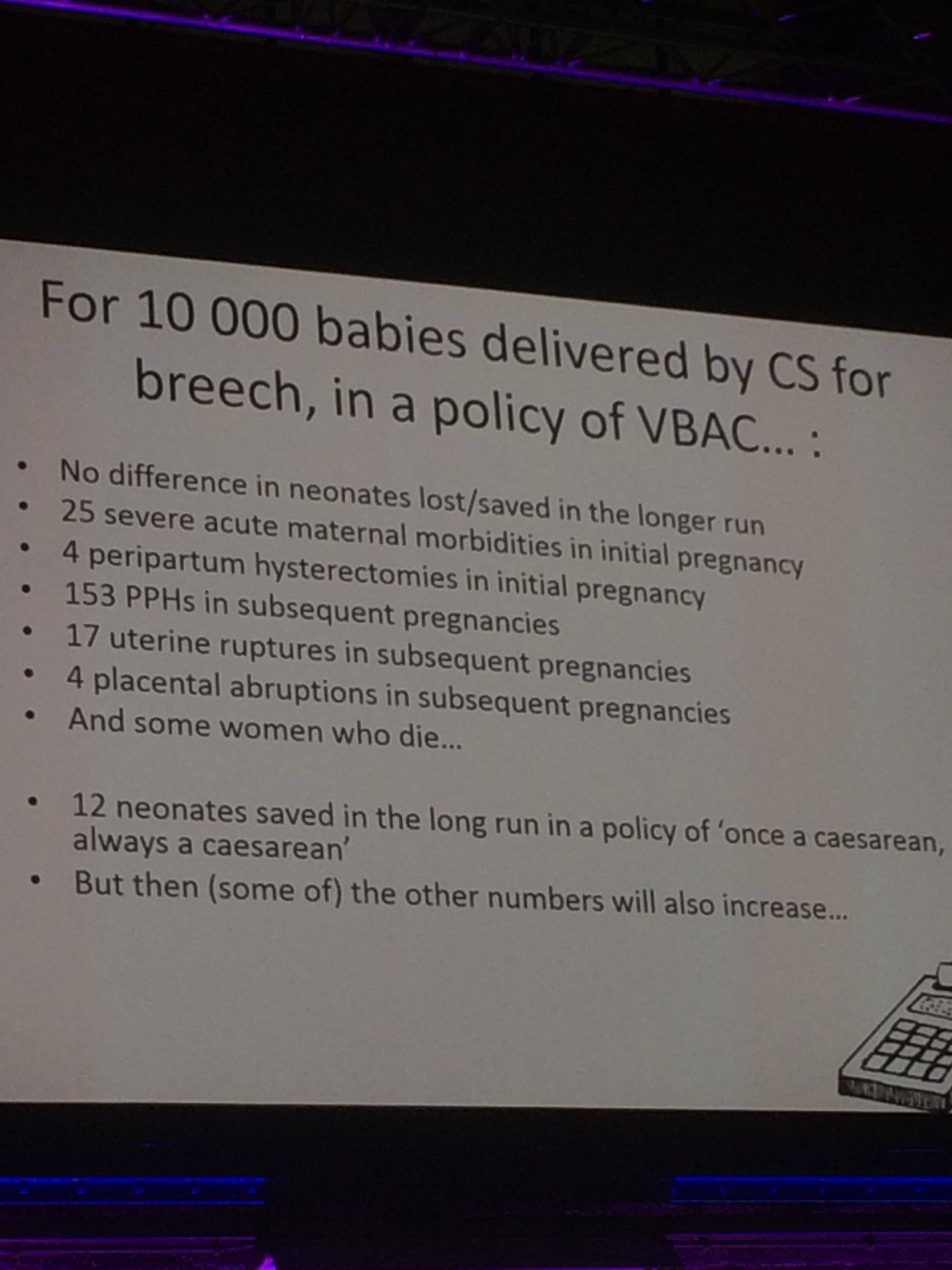
Thomas van den Akker, MD, PhD spoke profoundly on an unintended consequence of research adopted too quickly before it can be verified as was the TBT. His lecture was titled, “Who pays the price? (Foreign) women, future siblings”. He states that the number needed to treat (NNT) from the TBT is 338. (The NNT is the average number of patients who need to be treated to prevent one additional bad outcome). Meaning that 338 cesareans must be done to prevent 1 perinatal death. The conclusion that cesarean section is better, however, ignores the desires of the mother, future pregnancies and the rest of the world! In poorer countries the risks of surgical intervention are much higher than in the western world. Following the TBT guidelines would, in countries such as Tanzania, mean that a NNT of 338 would lead to 6 maternal deaths. In other words, to prevent one perinatal death the c/section all breeches model would kill 6 women instead. This is absurd and yet is considered the standard of care endorsed by many academicians and policy makers.
Finally, we ended the day with a discussion of preterm breech delivery. At 26 weeks about 25% of babies are breech. At 32 weeks it is 15% and by term it is the well-known number of 3-4%. Lester Bergenhenegouwen, MD PhD presented data that shows that there is no benefit to outcomes of fetuses <28 weeks or >32 weeks to be delivered by cesarean section. However with fetuses between 28-32 weeks there is a benefit with a perinatal mortality of 1.7/1000 for cesarean and 4.1/1000 for VBD. He states the overall the risk is small for mode of delivery. The major risk is the prematurity itself.
It was an interesting first day that raised as many questions as were answered. The 2 take home points for me were still related to the TBT. The gift that just keeps on giving. First, was Dr. Louwen’s comment about the flaw in comparing a standardized surgical procedure to the suboptimal methods of VBD used in the 1990s. The second was the unintended consequences of so rapidly adoptingthe recommendations of a single paper and its effect on training and maternal mortality worldwide.
In part 2 of this blog I will review the second day of lectures from the Amsterdam Breech conference and have some closing thoughts on Amsterdam, the state of scientific research in general and breech specifically and the importance of dialogue and collaboration.